Cerebral Palsy
CFI Family Featured in Magazine

Jared and Kathleen, along with their daughters Margot and Grace are featured in this July’s Greet Western Springs magazine.
Kathleen recently published a children’s book, “Stinky Mama,” promoting disability awareness and inclusion. Their favorite part of living in Western Springs is the friendly, supportive community, especially for Margot, who has cerebral palsy.
Read all about the Marcell Family’s journey in the July issue of Greet Western Springs Magazine!
Hillgrove Avenue Magazine Article

Feature Article About Working Together Chicago
Nora Dudley begins this article featuring WTC with the Herbst’s story:
In 1987, Justin Herbst was born ten weeks premature, and suffered a severe stroke. This led to a diagnosis of cerebral palsy–spastic quadriplegia, a permanent neuromuscular disorder and the most severe form of CP, limiting the ability to move the limbs, torso and face. Despite his diagnosis, Herbst’s mom Patti believed her son could become independent. A decade later and frustrated by a lack of improvement in the traditional medical therapy model, Herbst’s parents enrolled him in a Canadian program focused on conductive education…
What’s CFI Been Up To?
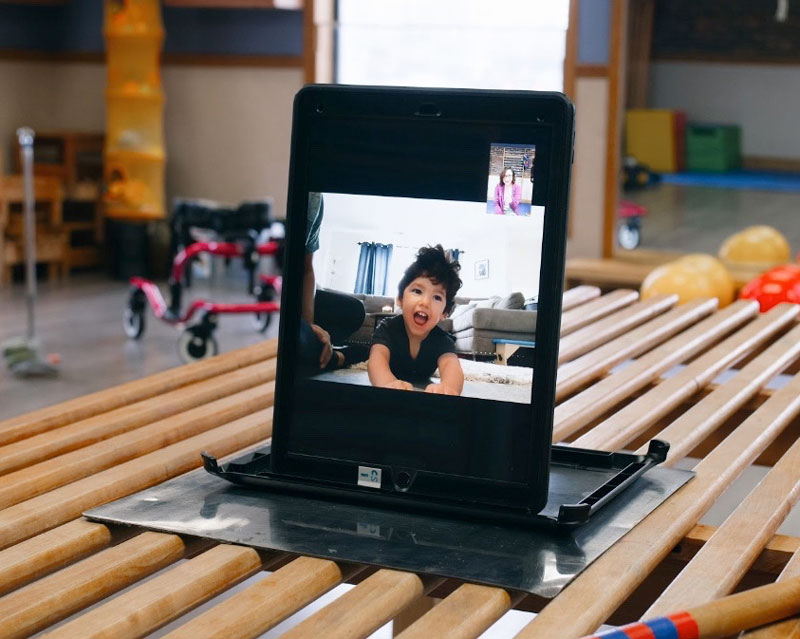
When the COVID-19 coronavirus health crisis closed the doors of Center for Independence our dedicated physical and occupational therapists, conductive education teachers and social worker opened their laptops, charged their smartphones and sprang into action! Our professional staff were ready to provide innovative, telehealth therapy services using social media outlets and video chat platforms!
Our hardworking staff immediately began (and continues!) to provide telehealth therapy services to more than 100 children and young adults with physical disabilities while our building is closed. To support the families during this pandemic, our therapy staff also developed home exercise programs and organized equipment lending for all families. We will continue providing telehealth therapy and social work services until Governor Pritzker declares it is safe for our doors to reopen.
Check out a short 90-second video of the talented Center staff delivering virtual PT, OT and CET services to children with physical disabilities:
During this time of crisis, people with cerebral palsy need access to vital healthcare services to breathe every breath, and step every step. The Center is using remote communication technologies to provide skilled healthcare intervention for those most at risk, so children and young adults with cerebral palsy stay active, remain healthy, and feel safe!
The Center fully understands the emotional and financial burden this crisis is having on our families. Our top priority is making sure that children and young adults with disabilities remain healthy and active. To help make that possible, the Center will not be charging families for telehealth therapy throughout the COVID-19 crisis.
The Center estimates that we will provide over $350,000 in charitable care teletherapy services to children and young adults with disabilities throughout the duration of our closure due to the pandemic.
How Can You Help?
You can change the lives of so many hardworking children and young adults with physical disabilities by making a donation. In this time of the unknown, you can make a difference in a way that works for you. If you donate now through June 1, 2020, your gift will be MATCHED by The Coleman Foundation up to $25,000!
Thank you for supporting the Center for Independence and the dedicated children and young adults we serve.
Announcing a New CFI Location

GRAND OPENING, JULY 17!
With the generous support of The Coleman Foundation and the community, the Center is thrilled to announce the opening of our new site located at 2701 W. 36th Pl., Chicago.
The space will include a large classroom and conference room for therapy programs, job training, parent education and community gatherings. Stay tuned for our grand opening in June!
Our heartfelt thanks to the talented staff of Studio 222 Architects, RTM Engineering, Bristol Design Group and John Lyle & Associates for donating so much of their time and expertise in making our new space a reality.
10 Principles of Neuroplasticity: Part 3
 Keep reading for part three, the final installment of the neuroplasticity series. Check out parts one and two if you haven’t read them yet! As a reminder, everything I write about here is found in the article, “Principles of Experience-Dependent Neural Plasticity: Implications for Rehabilitation After Brain Damage.”1
Keep reading for part three, the final installment of the neuroplasticity series. Check out parts one and two if you haven’t read them yet! As a reminder, everything I write about here is found in the article, “Principles of Experience-Dependent Neural Plasticity: Implications for Rehabilitation After Brain Damage.”1
6. Time matters
Different forms of change (plasticity) in the brain happen at different times during training.
The authors highlight how rehabilitation has different levels of efficacy at different points following a brain injury. Specifically, they discussed a study that found that rehabilitation provided 30 days after adults had strokes was far less effective, both functionally and neurologically than rehabilitation provided 5 days after the injury.
So what does this mean for children with CP? First of all, it means that therapy should be started as SOON as possible for babies with a suspected brain injury. Your child should be getting physical and occupational therapy while they are still in the NICU, and this should be continued when they are discharged home. Note that I say “suspected” injury intentionally: sometimes, it takes a while for a baby to be diagnosed with a neuromuscular disorder. This does not mean that the child doesn’t need therapy until they are diagnosed! The sooner therapy is started, the better their outcomes will be.
Secondly, puberty is also an important time to capitalize on neuroplasticity. Check out my previous article on CFI’s blog to read more about critical times for children with CP.
7. Salience matters
The training experience must be meaningful to the person in order to cause change (plasticity).
In every human brain, there’s a mechanism for remembering important things and forgetting less important things. Your brain isn’t able to contain photographic memories of every single experience you have in life, so it filters out which memories are more important to retain, and which ones you can live without.
This concept is true in rehabilitation as well: the experience needs to be meaningful to the child for neuroplasticity to be maximized. Kids need to have sufficient motivation and attention to the task at hand, and higher emotions and excitement help solidify motor learning. This is where conductive education truly excels because of the social context of therapy.
A great example is a popular activity sometimes used in class here called Body Bowling, which is the brainchild of our OT Josephine Boggs. In this activity, rolling is the main motor skill practiced, as kids compete to roll to knock over their bowling pins the fastest. This is a great therapeutic activity because it works on strengthening abdominal muscles, coordinating body parts to complete the movement, stretching shoulders, and so on. Kids don’t care about that, though. They care about winning the competition! It is amazing how much faster they roll during Body Bowling rather than alone as a warm-up activity. Making the activity fun and meaningful, or salient, to the child, not only increases their participation and enjoyment of the activity, but it makes stronger changes in the brain, too.
8. Age matters
Training-induced change (plasticity) occurs more readily in younger brains.
You may remember from part one of this series that I highlighted some good news about neuroplasticity: brains can change at any age! Well, here’s the bad news. While it’s absolutely true that brains at any age can undergo neuroplastic changes, it’s also true that changes are more robust at younger ages. This just serves to underscore the importance of beginning therapy as young as possible, and continuing throughout childhood and adolescence.
9. Transference
Change in function as a result of one training experience can even lead to learning other similar skills.
Researchers have found in a study of neuroplasticity, that after a group of people underwent training for a skill that involved the use of just one finger, neural pathways for use of the whole hand were strengthened. This finding indicates that it’s possible for one kind of training experience to enhance neural connections for other motor skills or body parts.
10. Interference
Brain changes (plasticity) that result in bad habits can interfere with learning good habits.
Neuroplasticity is usually used as a positive term, but not all neuroplastic changes are desirable. The authors of the article describe it well: “brain damage survivors may develop compensatory strategies that are easier to perform (“bad habits”) than more difficult but ultimately more effective strategies acquired through rehabilitation.” Learning those bad habits can make it harder for your brain to learn the “good habits” or better, more efficient, or safer movement patterns. The specifics of what are “good” or “bad” habits for kids with CP is highly specific and individualized to each child, so this is a good thing to ask your child’s therapist or CE teacher about.
As I did in part two, I want to pause for a moment to highlight what all of this has to do with conductive education. The truth is, any kind of experience or therapy will yield some sort of change in the brain, so for any therapist, doctor or clinic to claim to have a monopoly on neuroplasticity is just not true. However, based on the principles we just learned about, there are things you can do to really maximize on neuroplasticity to make those changes bigger and more meaningful. While conductive education indeed does address all ten principles, where I believe conductive education really stands out is with principles four, five and seven (repetition matters, intensity matters, and salience matters). You will be hard-pressed to find a commercially available therapy that provides greater repetition or intensity on a long-term basis than what is provided at the Center for Independence. In addition, the social context provides a rich environment ripe with opportunities to make movement meaningful to children, which provides the much-needed salience that was discussed above.
Congratulations on making it through the ten principles of neuroplasticity! I hope this leaves you with a better understanding of what neuroplasticity even is, and some of the most important factors in how to maximize neuroplasticity. Please leave any comments or questions on our Facebook page!
- Kleim, JA, Jones, TA. (2008). Principles of experience-dependent neural plasticity: Implications for rehabilitation after brain damage. Journal of Speech, Language, and Hearing Research, 51, S225-S239.